Thalassemia Patients Advocacy Group; (TPAG) celebrates its third anniversary on the World Patient Safety Day which is observed on 17 of September every year. The TPAG Group stresses on the importance of safe blood transfusion for those special patients undergoing a regular blood transfusion, like thalassemics, cancer patients and dialysis recipients who generally have a high risk of being exposed to transfusion-transmissible infections (TTIs). This poses a great threat on their lives.
Deepak Chopra, Co-Founder & President, Thalassemics India, expressed, “Thalassemics India is extremely proud to have undertaken the pioneering initiative of creating a body like TPAG. In doing this, we have fully empowered qualified and informed patient advocates to take forward the journey of not only protecting the interests of thalassemics but also of establishing the importance of patient participation in policy making. We stand right behind them in their path breaking efforts related to patient safety”
A recent report of NACO says 14,474 cases of HIV have been caused due to unsafe blood transfusion in India. It may be very much possible for a normal mother to return back home with a TTI like HCV, HBV or HIV after delivering a baby, as the patient have to undergo blood transfusion around the time of delivery. Therefore, blood is consistently used in a broad range of hospital procedures normally and such transmissions of TTIs can take place in patients easily undergoing a treatment.
As #TPAG renews its commitment to protecting the interests of #thalassemia patients and preventing #thalassemia, check out our journey of the past THREE years! #HappyBirthdayTPAG #PatientAdvocacy #Healthcare @thalassemic @thalassaemiaTIF pic.twitter.com/ELVNHwrXQ8
— Thalassemia Patients Advocacy Group (@pagthals) September 16, 2020
Anubha Taneja-Mukherjee, a legal & policy advocacy professional and Member Secretary of TPAG commented, “Safe blood is one of our focus areas and we are committed to partnering policy makers in propagating, implementing and advocating best practices related to blood in India. To achieve the objective, all aspects of blood safety, including blood donation, transfusion, and screening technology will need to be covered. In our efforts, we will try to address some difficult questions- what it costs to prevent a TTI in comparison to treating one (and, TTIs like HIV are incurable!)?; Can a patient getting transfusion in Jharkhand get a different quality of blood than one sitting in Bengaluru? Is there a golden standard for blood screening across India or a mechanism that allows one blood bank to pick a screening method different from another blood bank and do blood banks need to keep in mind repeat recipients of blood while making these choices? And, should patients move from a safer technology to a less safe technology due to compulsions of Covid-19?
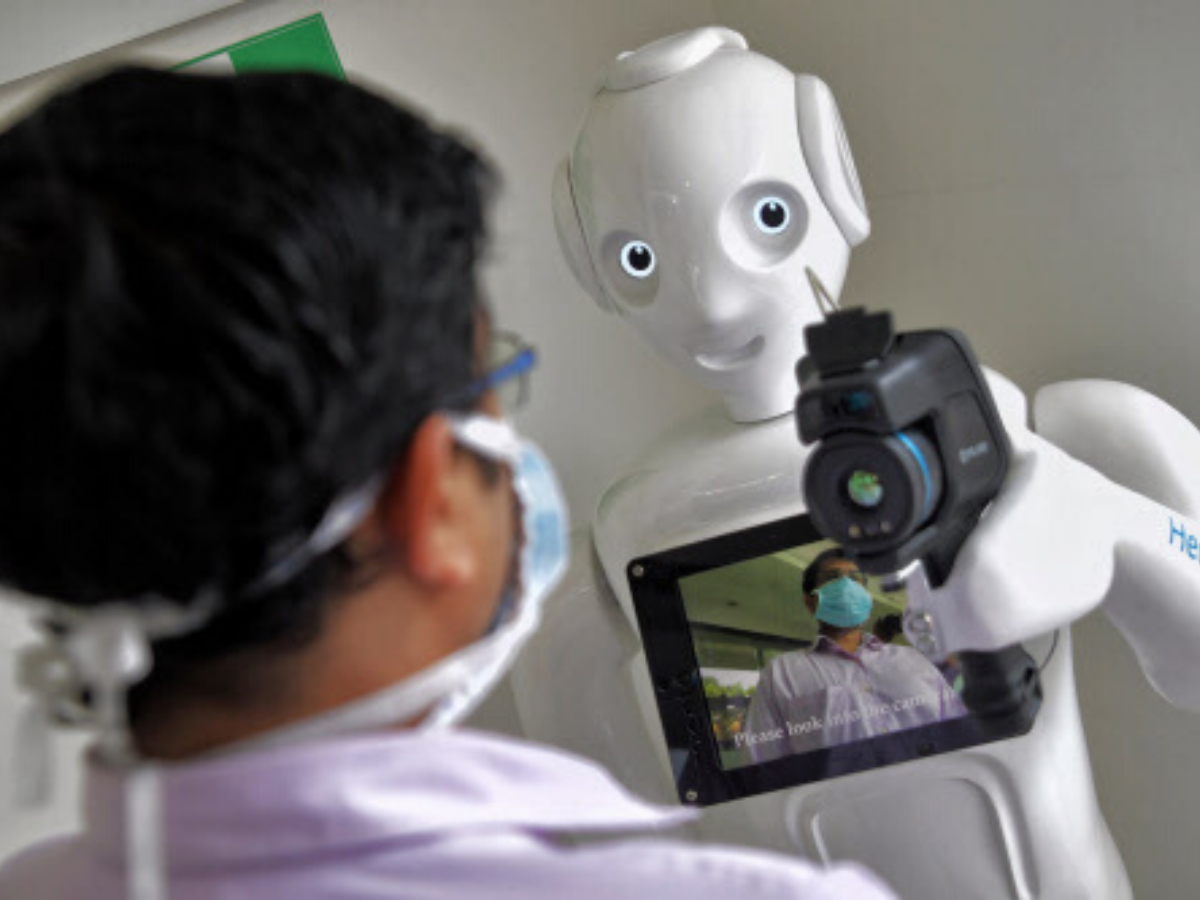
While, Dr R N Makroo President Indian Society of Transfusion Medicine Regional Director Transfusion Medicine Medeor Group of Hospitals Delhi NCR, expressed on the point of repeat recipients and said, ““Blood Transfusion is lifeline for Thalassemia patients and accordingly they should receive the safest possible Blood. Although there is no Zero risk blood but by adopting best transfusion strategies which includes provision of blood from regular repeat voluntary non remunerated blood donors. Latest and best testing technologies for infectious marker screening (HIV, HBV& HCV) Including NAT testing to narrow the window period transmissions of these infections. Type & Screen Policy including provision of red cell antibody Screening & identifications If antibody screen is positive then provision to provide red cell antigen negative blood. In order to have safe blood of uniform standards for all patients the Country needs Centralized blood collection & testing”
What is the focus of Government?
#OneIndiaOneBlood is a slogan of Government of India and its focus on TTIs is apparent because it has come up with the National Viral Hepatitis Control Programme, which is in line with the Sustainable Goals. Moving towards “zero-risk” transfusion of blood is critical for the success of this Programme. Therefore a maintaining a stringent guideline for testing and policy implementation is very much required. Turing to that, all these need a data data-driven impact assessment of various clinical test combinations, algorithms and thorough cost-benefit analysis to arrive at a combination suitable which is practical for India.
On the part of treatment of TTIs possibility of prevention can be done with strict implementation of guidelines related to blood transfusion should be used by further harmonising and mandating uniform screening methodologies across India.
India has seen an increase in blood collection (from 9.8 million units in 2012-12 to 11.45 million in 2017-18) and currently has over 2800 blood banks in the private and public sector. However, India still has blood shortage of ~1.95 million units, so the first step to ensure safe blood is the Voluntary blood donation. Whereas, the launch of E-RaktKosh by MoHFW is a great step towards this direction.
Also, India needs to assess the superiority of Nucleic Acid Testing technology (NAT) method as a safe option for blood screening since it ensures 99.99% blood safety.
What is the insight of WHO on this?
WHO recommends, that blood requirement of a country’s population should be between 1%-3%. The blood shortage during COVID-19 has made it more difficult therefore there is a complete requirement of boosting up the dose for Voluntary blood donation. Voluntary blood donation can be also conducted with other recommended practices and tests in order to make the blood safe.