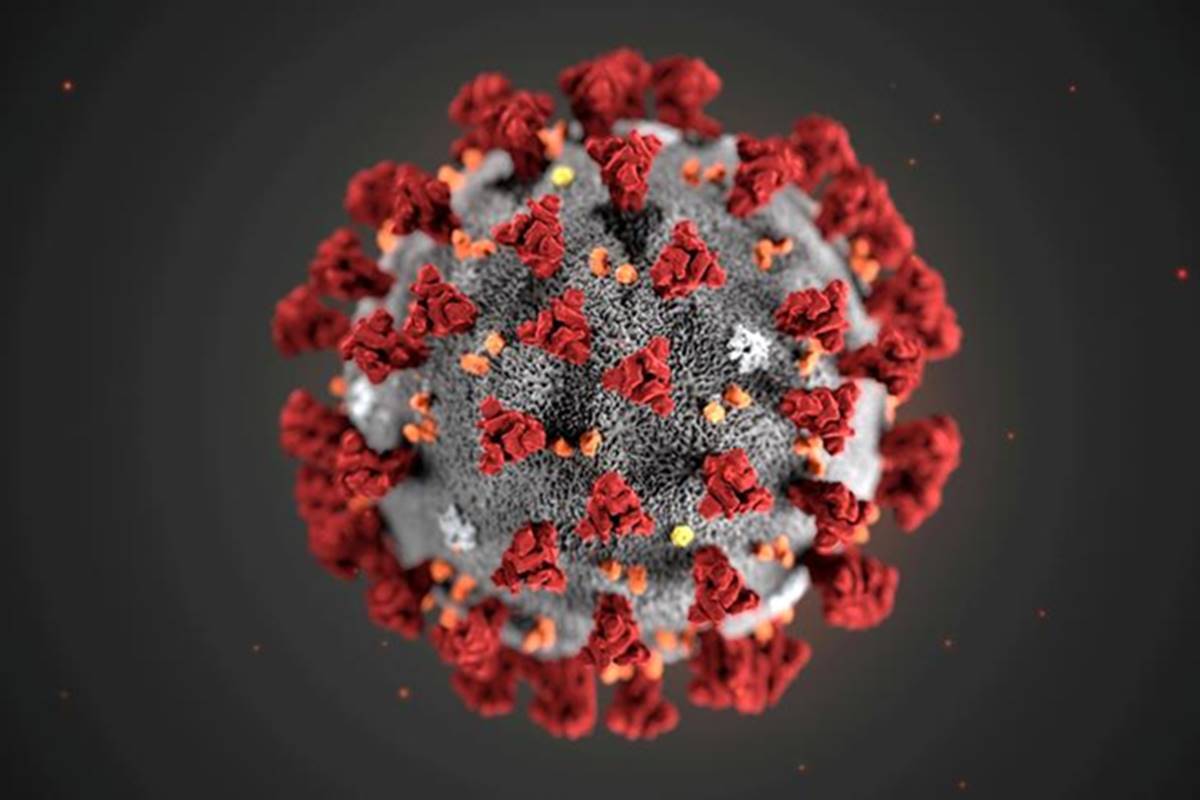
A new report, published in the medical journal Lancet, shows that there is consistent, strong evidence that the SARS-CoV-2 virus, which causes COVID-19, is principally transmitted through the air.
Six experts from the UK, USA, and Canada, including Jose-Luis Jimenez, a chemist at the Cooperative Institute for Research in Environmental Sciences (CIRES) and the University of Colorado Boulder think that this is the reason why public health measures fail to treat the virus as predominantly airborne leave people unprotected and allow the virus to spread.
“The evidence supporting airborne transmission is overwhelming, and evidence supporting large droplet transmission is almost non-existent,” Jimenez said.
“It is urgent that the World Health Organization and other public health agencies adapt their description of transmission to the scientific evidence so that the focus of mitigation is put on reducing airborne transmission.”
“This report is not dramatically new but what it’s talking about is that the virus is airborne that means the transmission can be done by air. Previous coronaviruses behaved the same way. For Covid-19, experts had been warning that the virus stick to the surfaces and they stressed the importance of surface cleaning and hand hygiene to contain the spread of the virus. But what Lancet is saying that surface transmission is not an issue as much as airborne, therefore one has to do social distancing and wear masks. This is an important revelation, but that does not mean we should lower our guard stop maintaining hand hygiene. Hand hygiene should not be given any less importance.” Dr. Pravin Khilnani Senior consultant Peaditrics Madhukar Rainbow Hospital, Delhi says, while talking to HealthWire.
The published research has been reviewed by the team of experts led by the University of Oxford’s Trish Greenhalgh in which 10 lines of evidence were identified to support the predominance of the airborne route.
At the top of their list: Super-spreader events such as the Skagit Choir outbreak, in which 53 people became infected from a single infected case.
Studies have confirmed these events cannot be adequately explained by close contact or touching shared surfaces or objects.
Moreover, transmission rates of SARS-CoV-2 are much higher indoors than compared to outdoors, and transmission is greatly reduced by indoor ventilation.
The team noted research estimating that silent (asymptomatic or presymptomatic) transmission of SARS-CoV-2 from people who are not coughing or sneezing accounts for at least 40 percent of all transmission.
This silent transmission is a key way COVID-19 has spread around the world, “supporting a predominantly airborne mode of transmission,” according to the analysis.
The researchers also cited work demonstrating long-range transmission of the virus between people in adjacent rooms in hotels; people who were never in each other’s presence. By contrast, the team found little to no evidence that the virus spreads easily via large droplets, which fall quickly through the air and contaminate surfaces.
Lead author Greenhalgh said, “We were able to identify and interpret highly complex and specialist papers on the dynamics of fluid flows and the isolation of the live virus.”
“While some individual papers were assessed as weak, overall the evidence base for airborne transmission is extensive and robust. There should be no further delay in implementing measures around the world to protect against such transmission.”
The new work has serious implications for public health measures designed to mitigate the pandemic. First, “droplet measures” such as handwashing and surface cleaning, while not unimportant, should be given less emphasis than airborne measures, which deal with inhalation of infectious particles suspended in the air.
Someone can potentially be infected when they inhale aerosols produced when an infected person exhales, speaks, shouts, sings, or sneezes if an infectious virus is primarily airborne.
So airborne control measures include ventilation, air filtration, reducing crowding and the number of time people spend indoors, wearing masks whenever indoors (even if not within 6 feet or 2 meters of others), attention to mask quality and fit, and higher-grade PPE for healthcare and other staff when working in contact with potentially infectious people.