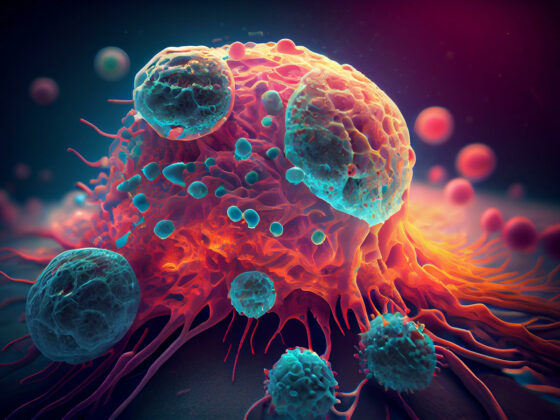
How do ovarian cancer cells interact with blood vessels and platelets? Currently, researchers understanding of the this interaction is confined to this: platelets are one of the initiators of ovarian cancer metastasis.
A collaborative research, involving scientists from the Department of Biomedical Engineering and the Department of Medical Physiology in the College of Medicine and the Departments of Gynecologic Oncology and Cancer Biology at MD Anderson Cancer Center, has tried to find led to the introduction of the platelets to the ovarian tumor cells.
The researchers, including an Indian origin scientists Dr. Abhishek Jain, found that tumors break the blood vessel barriers so that they can communicate with the blood cells, such as platelets.
The study published in the in the journal Blood Advances, is significant as it has viewed the relationship between blood vessels and platelets in animal models. Instead they brought a new solution to the table: organ-on-a-chip research.
Organs-on-a-chip are microfluidic medical devices the size of a USB drive. The team designed on the OvCa-Chip to give researchers an easier window to view the biological processes between tumors and platelets.
What is this organ-on-a-chip research?
Dr. Abhishek Jain, assistant professor in the Department of Biomedical Engineering and the Department of Medical Physiology in the College of Medicine, explained it :a microenvironment where ovarian tumor cells can be co-cultured along with their blood vessels, and then they can interact with blood cells”.
Better understanding of these understanding will bring the researchers a step closer to find the efficacy of drugs. Once they know the effect of drugs on these interactions, they will move forward in right direction.
Viewing the interaction between tumors and blood vessels on the OvCa-Chip led the researchers to an extraordinary result — the tumor cells systematically broke down the endothelial cells, which are the barrier that lines the interior surface of blood vessels and prevents exterior interaction with blood cells.
Once this barrier was gone, blood cells and platelets entered the tumor microenvironment and could be recruited for metastasis.
Anti-vascular drugs could be considered along with anticancer treatments. A benefit of the organ-on-a-chip is that it can also test these novel drug treatments and drug combinations.
Although ovarian cancer is the fifth-leading cause of death from cancer in women, scientists don’t know on how it forms.
A new study published in Nature Communications suggests that a microRNA—a molecule made by cells to turn genes on and off—may help kick-start a type of ovarian cancer called high-grade serous ovarian cancer.
The current thinking is that ovarian cancer starts in fallopian tube cells that have a few gene mutations. Those abnormal cells eventually turn into a precursor of cancer, or precancer. Years later, the precancer becomes full-blown ovarian cancer.
But scientists don’t know what drives the transition from mutated fallopian tube cells to precancer to ovarian cancer.