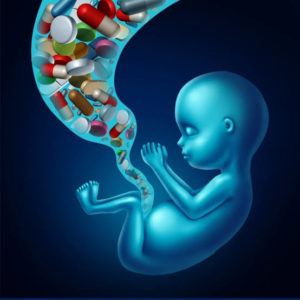
The primary source of Hepatitis B (HBV) infection, a bigger killer than HIV/ AIDS, malaria and tuberculosis combined, is to be found among infected pregnant women, who are at a very high risk of passing the virus to their children.
Dr Subhash Gupta, Hepatologist, Max Super-specialty Hospital, Saket, says that a person infected with HVB at a younger age or during the time of birth carries it life-long and can manifest it anytime. Dr Anil Arora, Senior Gastroenterologist, Sir Ganga Ram Hospital, says that a HBV infected baby has a 95 per cent chance to live with the virus throughout his/her life and would be prone to compromised parameters and infection. Both doctors say that if the infection is contracted during adulthood, there are 95 per cent chances that it can get cleared within six months.
“The baby’s weak immune system allows HBV to survive”, says Dr Arora. Not only that, the virus can stay silent and asymptomatic even for decades until carriers develop conditions in young adulthood or mid-life with decompensated cirrhosis, liver failure or hepatocellular carcinoma. Dr Arora admits to treating several cases in his clinic where people have been diagnosed with serious liver ailments after several years of infection. Around the world, about 300 million people are infected with hepatitis B virus and 90 per cent of them don’t even know they have it, says a study published in the Lancet Gastroenterology & Hepatology journal on March 26, 2018.
At 40 million, India has the maximum number of people infected with the Hepatitis B virus (HBV) after China, of which 1-2 per cent die every year. Up to 90 per cent of babies born to carrier mothers become carriers themselves and are at a very high risk of developing chronic liver disease at a younger age.
So how can we prevent transfer of the virus? “The HVB vaccination is very effective. Pregnant women should get tested for HVB and if she is positive, the child should be vaccinated soon after birth”, says Dr Gupta.
Dr Gupta says if the carrier pool (HVB-infected pregnant women) can be screened and treated, then the HVB could be effective as the next generation gets infection from mothers and, of course, from contaminated blood, infected syringe, unsafe sex practices and so on. Dr Gupta says the whole focus is on universal immunisation for HVB, that may not be very cost-effective but if all pregnant women come under the loop of mandatory screening, treatment and vaccination of new-born babies, then elimination could be achieved easily.
Dr Arora says India has made screening of pregnant women mandatory nearly 20 years ago. However, it loses its relevance in areas where institutional delivery is low. According to the National Family Health Survey (NFHS-4), there is a gap of nearly 22 per cent in institutional delivery in the country.
The recently-launched National Viral Hepatitis Control Programme (NVHP) aims at eliminating viral hepatitis. Apart from other measures, the programme also focusses on screening of pregnant women for HVB in places where institutional delivery is less than 80 per cent to ensure provision of birth dose HVB vaccination and Hepatitis B immunoglobulin, if required. This can prevent the next generation from being grappled by chronic hepatitis, cirrhosis and hepatocellular diseases.