New Delhi, 07 December 2024: A new study has uncovered a significant connection between ovarian removal and an increased risk of Alzheimer disease in women. The findings, published in a prominent medical journal. Highlight the long-term cognitive health risks associated with surgical menopause, particularly in younger women. This research is a critical addition to the growing body of evidence linking hormonal changes to neurodegenerative diseases.
Hormonal Role in Cognitive Health
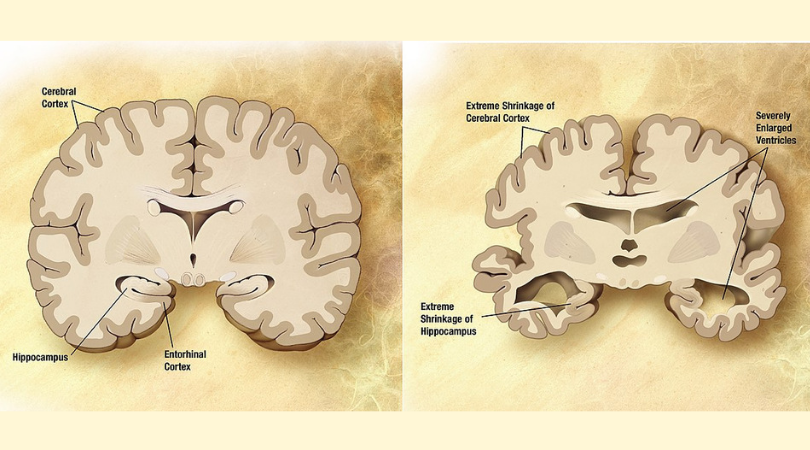
The study emphasizes the importance of estrogen in maintaining brain health. Estrogen, a hormone produced by the ovaries, plays a protective role in the brain by supporting neuronal function and reducing inflammation. When ovaries surgically removed, known as oophorectomy, estrogen levels drop significantly, especially if the procedure performed before natural menopause. This abrupt hormonal change may leave the brain vulnerable to damage over time. Increasing the risk of Alzheimer’s and other forms of dementia.
Key Findings of the Study
The research analyzed medical records of thousands of women who had undergone oophorectomy. Comparing their cognitive health outcomes to those who retained their ovaries. The data revealed that women who had both ovaries removed. Before the age of 45 were at the highest risk of developing Alzheimer’s disease later in life. The risk particularly pronounced in those who did not undergo hormone replacement therapy (HRT) to counteract the loss of estrogen.
The researchers noted that the timing of HRT initiation also played a crucial role. Women who began HRT shortly after surgery appeared to have a lower risk of Alzheimer’s compare to those who delay or avoid the therapy altogether. These findings suggest that early hormonal intervention could mitigate some of the cognitive risks associated with oophorectomy.
Implications for Women’s Health Decisions
The study underscores the need for careful consideration before opting for ovarian removal. Particularly for non-cancerous conditions such as endometriosis or benign ovarian cysts. While the procedure is sometimes necessary to address certain health concerns. It is essential for women and their healthcare providers to weigh the long-term risks alongside the immediate benefits.
Women undergoing oophorectomy for cancer prevention, such as those with BRCA gene mutations, face a complex decision. For these individuals, the benefits of reducing cancer risk often outweigh the potential cognitive risks. However, the study highlights the importance of discussing HRT as part of post-surgical care to help offset the impact of estrogen loss on brain health.
Alzheimer’s Risk in Women
Alzheimer’s disease disproportionately affects women, with nearly two-thirds of Alzheimer’s patients being female. While the reasons for this gender disparity not fully understood. Hormonal changes during menopause thought to be a contributing factor. This study adds to the growing understanding of how estrogen loss can accelerate cognitive decline, particularly in women who experience premature menopause due to surgery.
Recommendations for Women and Healthcare Providers
Based on the study’s findings, researchers urge healthcare providers to discuss the potential long-term risks of ovarian removal with their patients. Women who undergo the procedure should informed about the benefits of HRT and the importance of early initiation to support cognitive health. Regular cognitive assessments and lifestyle interventions. Such as a healthy diet, exercise, and mental stimulation, also recommended for women at higher risk of Alzheimer’s.
Read Also – WHO Grants Prequalification to Molecular Diagnostic Test for Tuberculosis
The study provides crucial insights into the link between ovarian removal and Alzheimer’s risk, emphasizing the need for informed decision-making and proactive healthcare strategies. While oophorectomy may be unavoidable in some cases, addressing the hormonal changes through HRT and lifestyle modifications can help mitigate the associated cognitive risks. These findings highlight the broader implications of hormonal health in women’s overall well-being, encouraging both patients and healthcare providers to adopt a holistic approach to care.