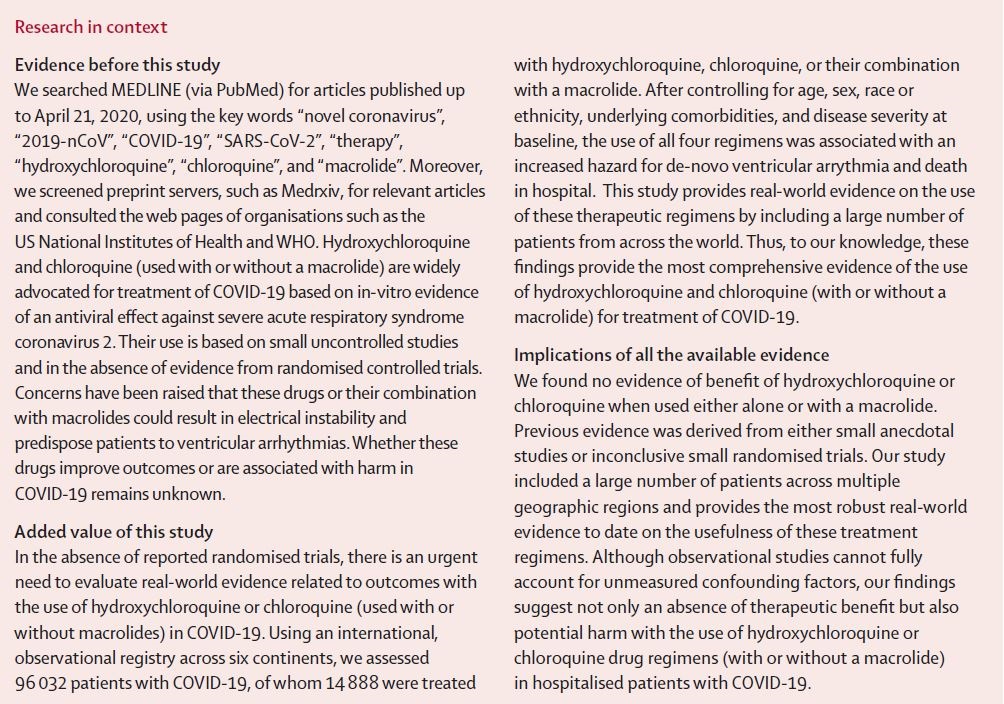
According to a new study published in The Lancet, Hydroxychloroquine or chloroquine, often in combination with a second-generation macrolide, are being widely used for treatment of COVID-19, despite no conclusive evidence of their benefit.
Although generally safe when used for approved indications such as autoimmune disease or malaria, the safety and benefit of these treatment regimens are poorly evaluated in COVID-19.
The Lancet did a multinational registry analysis of the use of hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19. The registry comprised data from 671 hospitals in six continents.
It included patients hospitalised between Dec 20, 2019, and April 14, 2020, with a positive laboratory finding for SARS-CoV-2. Patients who received one of the treatments of interest within 48 hour of diagnosis were included in one of four treatment groups (chloroquine alone, chloroquine with a macrolide, hydroxychloroquine alone, or hydroxychloroquine with a macrolide), and patients who received none of these treatments formed the control group.
The study analysed data from nearly 15,000 patients with Covid-19 receiving a combination of any of the four drug regimens and 81,000 controls. Treatment with these medications among patients with Covid-19, either alone or in combination with macrolide antibiotics, was linked to an increased risk of serious heart rhythm complications.
Professor Dr Frank Ruschitzka, director of Heart Centre at University Hospital Zurich, who co-authored the study, said that treatment with the antimalarial drug chloroquine, or its analogue hydroxychloroquine (taken with or without antibiotics azithromycin or clarithromycin), offers no benefit to patients of Covid-19.
“Several countries have advocated the use of chloroquine and hydroxychloroquine, either alone or in combination, as potential treatments for Covid-19. Justification for repurposing these medicines in this way is based on a small number of anecdotal experiences that suggest they may have beneficial effects for people infected with the SARS-CoV-2 virus. However, previous small-scale studies have failed to identify robust evidence of a benefit and larger, randomised controlled trials are not yet completed. However, we now know from our study that the chance that these medications improve outcomes in Covid-19 is quite low,” Dr Frank added.
Patients for whom one of the treatments of interest was initiated more than 48 h after diagnosis or while they were on mechanical ventilation, as well as patients who received remdesivir, were excluded.
The main outcomes of interest were in-hospital mortality and the occurrence of de-novo ventricular arrhythmias (non-sustained or sustained ventricular tachycardia or ventricular fibrillation).