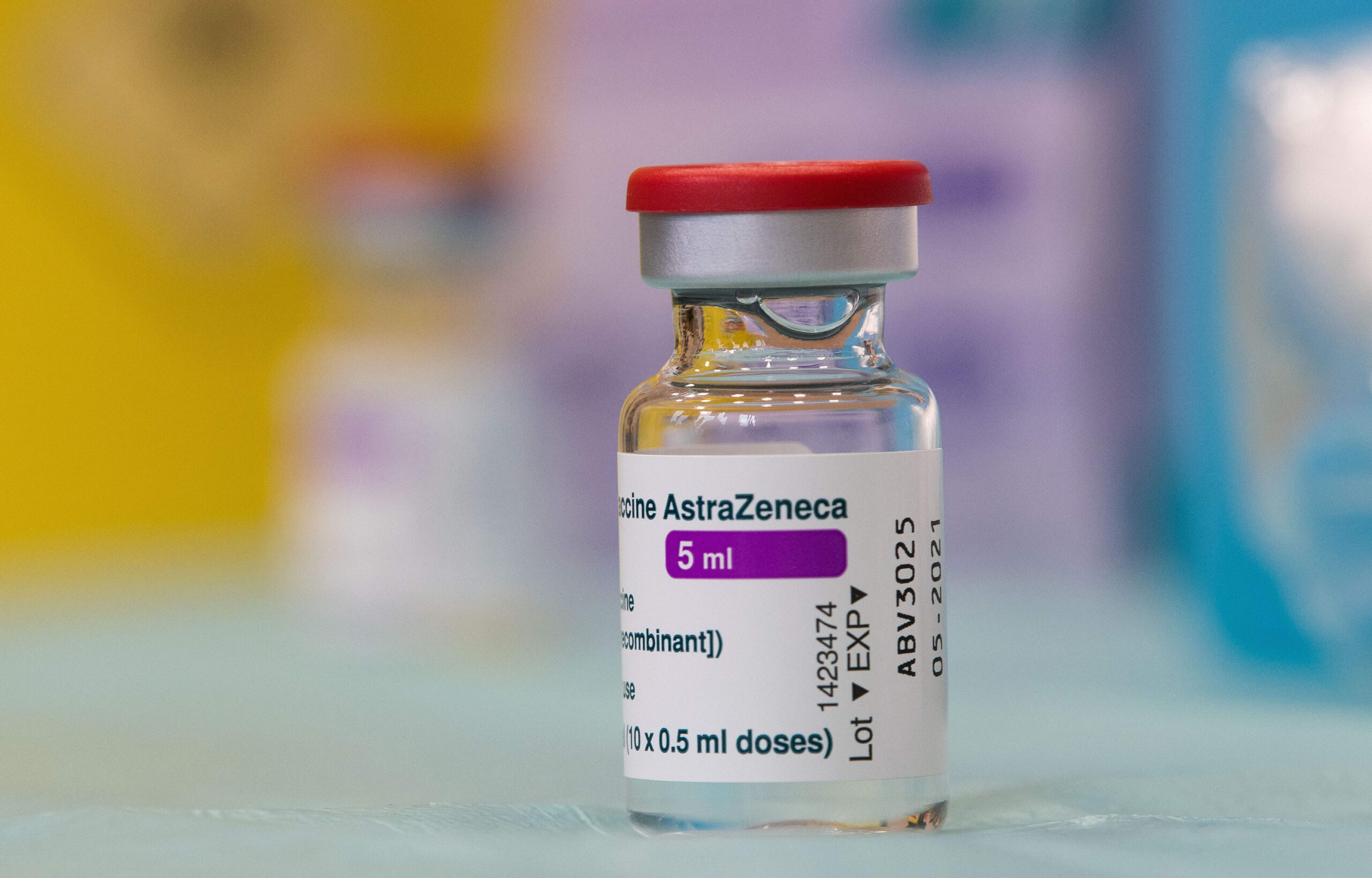
The UK drug regulator found an extremely rare nerve-damaging disorder, Guillain-Barre syndrome (GBS), as a very rare side effect of the AstraZeneca COVID-19 vaccine, updates on the agency’s website showed on Thursday. Medicines and Healthcare products Regulatory Agency’s (MHRA) decision comes after the European medicines agency added GBS as a possible side-effect last month.
New Antibody Treatment Could Offer Up To 18 Months’ Protection Against Severe Disease
A new treatment could soon help cover people from developing severe COVID. AstraZeneca has just released results from a phase 3 clinical trial – the final stage of testing before medicine is authorised – that suggest its new COVID treatment, AZD7442, is effective at reducing severe complaints or death in non-hospitalised COVID cases.
The treatment contains antibodies, which are generally produced naturally in response to a COVID infection or vaccination. They work by recognising specific corridors of SARS-CoV-2 – the contagion that causes COVID – and either attack these directly or bind to them to stop the contagion from working and flag it for destruction by other corridors of the vulnerable system.
After they have done their job of clearing the contagion, the antibodies remain in the body for a period of time, making up part of our immunological memory. However, they can vault into action, If what they target is encountered again.
The new treatment, AZD7442, uses special antibodies called monoclonal antibodies. These are antibodies produced in a lab that imitate the body’s natural defences – in this case mimicking the vulnerable system’s response to COVID. Instinctively developing antibodies to fight complaint is not a new fashion. This technology is formerly used to treat numerous conditions, including leukaemia, bone cancer and lupus. In fact, this is not indeed the first time the fashion has been used for COVID. The first COVID monoclonal antibody treatment was approved in the UK in August 2021.
How does AstraZeneca’s treatment work?
AZD7442 is a blend of two monoclonal antibodies – tixagevimab and cilgavimab – that are designed to reduce the inflexibility of a SARS-CoV-2 infection and so help people from getting oppressively ill. Both of these antibodies bind to the different corridors of contagion’s shaft proteins, which cover its external face and are what the contagion uses to infect cells. It’s allowed that attaching to these proteins is what gives the drug its effect, as this stops the contagion from being suitable to get inside cells and reproduce.
The two monoclonal antibodies in the blend are grounded on antibodies taken from cases who survived COVID. Scientists at AstraZeneca took blood samples from cases and insulated vulnerable cells called B cells, which are the antibody manufactories of the mortal body. They also grew further of these B cells in the lab, and used them to make large amounts of the two antibodies, which they had linked as specifically targeting the coronavirus’s shaft protein.
But the crucial difference between this and other antibody- grounded treatments is that in AZD7442, the antibodies have been modified so they stay in the body for longer. Studies using also modified antibodies against another respiratory contagion – respiratory syncytial contagion – have shown that this approach gives long- term protection, with the modified antibodies having triple the continuity of conventional antibodies. It’s hoped that a single cure of AZD7442 could offer 12 to 18 months protection from severe COVID, though we’ll have to stay to see exactly how long protection lasts.